The mask I wear: part 2
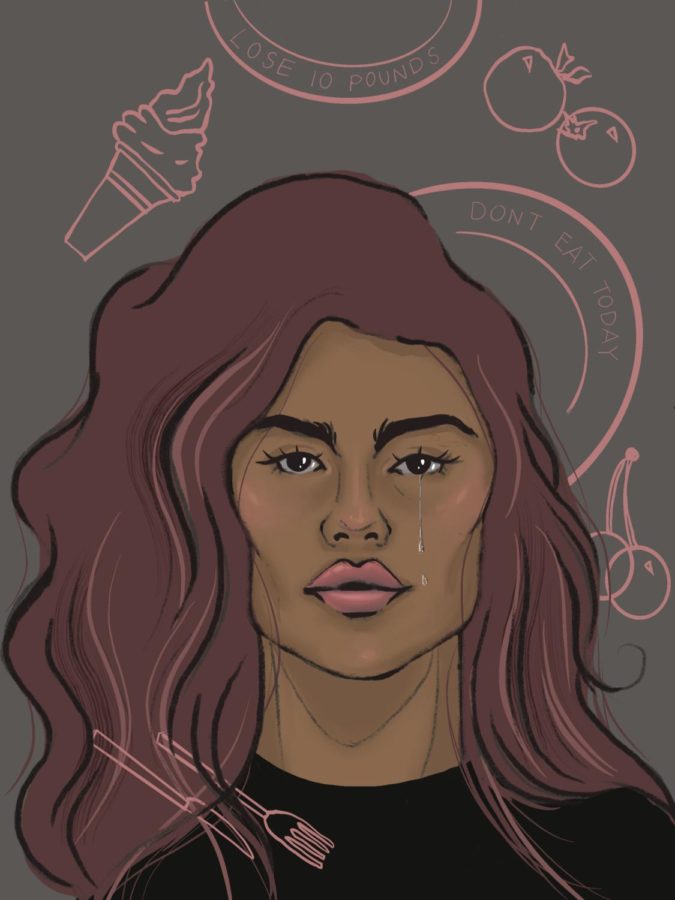
Staff writer, Meileen Arroyo, shares her experience with Anorexia Nervosa.
March 10, 2023
Important: This is a continuation of part 1 of the series ‘The mask I wear.’ Go read part one before you read this story if you haven’t read it yet. This story contains sensitive topics that may be emotionally triggering for some. Topics include eating disorders, eating behaviors, and suicidal ideation. If you are currently struggling with mental health and feel as if this story will induce negative thoughts and behaviors please click out for your own well-being. My intention is not to glorify eating disorders. I am solely sharing my own experience.
Friday – March 18th, 2022
I have an appointment at the Providence eating disorder clinic for adolescents soon. The nerves are starting to set in. My biggest fear is getting denied or told that I’m fine or don’t meet the requirements to be diagnosed. I don’t look like I have an eating disorder. If I told people they wouldn’t believe me because I’m not skinny. I don’t look “anorexic” and I never did. I hate that I’m slowly getting better. If I don’t have this eating disorder then I have nothing. It gives me life, it makes me be in competition with myself and I secretly love it.
– M
After I was let go as a patient from my first therapist, my mom called the Providence Hospital Eating Disorder Program for Adolescents to schedule an evaluation appointment. The appointment was scheduled for March 28th and would last about 2 hours. I was frustrated that I would continue being in therapy after being let go. In all honesty, I didn’t want to go back to having weekly therapy sessions, I wanted to forget that this ever happened and move on with my life. At this point, I didn’t believe I had a problem. The praise I received from my family and primary care provider on my weight loss made me believe I didn’t have an eating disorder. I thought that because I was at a medically “healthy” weight and never got to the point of being underweight for my height, that meant I didn’t have an eating disorder. I thought that eating disorders had a specific “look” and to me that meant being thin.
March 28th came around, I sat in a small waiting room with my mom listening to the instrumental music that played through the speakers. I stared blankly at the sheet of paper that required me to write down everything I ate in a day. I wrote down the following: an apple and peppermint tea for breakfast, salmon and vegetables for dinner, exactly 12 cashews, 1/2 cup of grapes, and water throughout the day. I was surprised at the amount of food I consumed. Seeing everything I ate in a day written down on a piece of paper made me realize that maybe there was something wrong but my internal voice powered over this thought and inevitably won the fight. Once my name was called I said goodbye to my mom and followed a lady back to an empty room. The first step was recounting the story on how I developed an eating disorder. I answered question after question as truthfully as I could and after 2 hours of the evaluation my mom was called over to give her perspective. From beginning to end my mom told the events from her point of view, she brought attention to some things I left out from my portion of the evaluation. From across the table, the lady was writing down additional notes and occasionally nodded her head and raised her eyebrows when something intense was mentioned. Finally, when the evaluation was done the lady left the room and my mom and I were left alone. During these five minutes none of us said a word, we simply sat in silence and waited for the lady to return. “Based on the evaluation you exhibit symptoms of Anorexia Nervosa.” Two women stared at me as I took in the official diagnosis. They told my mom and I that the adolescent program would be a good fit for me and that I could start as soon as I got my blood work results from my primary care provider. Estimating that everything worked out fine I could start at the beginning of April. However, there was a slight problem. The program consisted of partial hospitalization/intensive outpatient treatment. That meant that Monday through Friday I would be at the hospital from 12 PM to 4 PM for a total of 8-9 weeks. If I started treatment in April, I would only be able to attend one class every school day because I would have to leave early for treatment. This was a problem for me, I didn’t want to miss the rest of my junior year or jeopardize my grades. The only other option was to spend my entire summer in eating disorder treatment. As much as this sounded unappealing to me, I didn’t have any other choice. That same day, I was put on the wait-list for summer treatment and it was time for me to mentally prepare for what was soon to come…recovery.
On the last day of my junior year, my mom gave me the news that I would be starting treatment on June 24th. It was official. I would be entering a world I did not want to explore. I would be spending all my summer trapped in a hospital instead of hanging out with my friends or touring college campuses like I had planned. After my mom told me the news, I fell into a deep depression. (**Content warning: mention of suicidal thoughts and self harm) I was angry at my mom for confirming my enrollment without speaking to me first. All my emotions exploded and my suicidal thoughts worsened. “You can end this and you won’t have to go to treatment.” My logical side knew that suicide wasn’t the answer. I knew that the real me didn’t think this way, this was my distorted alter ego talking to me. This was shadow, not Meileen. Instead of attempting suicide, I resorted to my dangerous coping mechanisms: extreme restriction and self inflicted injury. I punched, hit, and pinched myself countless times leaving huge bruises of all sorts of colors. I used myself as my own punching bag because I was so frustrated with the world. Now looking back on this, part of me is embarrassed for admitting that I used to engage in self-harm, but now I’ve come to realize that I’m not the only one that engaged in these sorts of behaviors to cope with extreme feelings. There’s a dangerous underlying secrecy to self-harm that causes people to feel shameful towards it, but in order to heal, one has to let the shame and guilt of self-harm go. The starvation, punching/pinching, negative self talk, and extreme exercise were my coping skills but these behaviors were also forms of self-harm.
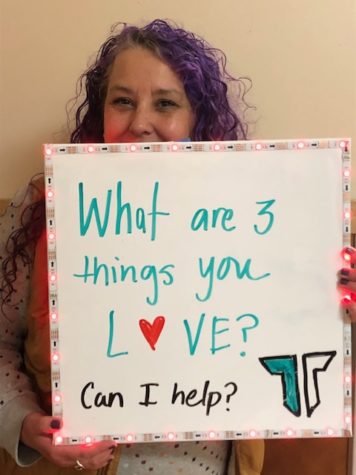
June 24th was the day I started eating disorder treatment. While sitting in the waiting room, I could feel the other patients’ eyes on me. They tried their hardest not to look at me, I could tell they were curious as to who this new addition to the program was. At 12:15 PM they took all of us back into the clinic and we broke off into two groups: purple (my group) and red. After I sat down at my own designated table, I was instructed to lay out my lunch so the dietitian could review it and make sure it met the guidelines. My “healthy” lunch that consisted of a salad with romaine lettuce, cucumber, lemon juice (as the dressing), and a side of apple slices wasn’t enough. The dietitian added an english muffin and peanut butter to my lunch to complete the necessary caloric value. Tears welled in my eyes as I thought about eating the english muffin, let alone eating lunch for the first time in two years. Everyday before eating lunch, patients participate in something called “intentions.” Intentions was a time where the patients could vocalize their meal completion goal and one challenge regarding lunch time (EX: Intention is to finish 80% of my meal and a challenge I have is that I’m anxious about eating my sandwich). I remember my first intention was 50% and my challenge was the english muffin. During lunch time, we played games and asked questions to get to know each other. These activities served as distractions and helped us to not be so fixated on the food in front of us. Once lunch ended, the dietitian came back in the room and scanned everyone’s meal. The dietitian would say a percentage out loud and that percentage was your meal completion for the day. If you were unable to finish your lunch, the meal completion percentage was used to measure how much boost you would have to drink in order to supplement the uneaten calories from your lunch. I stared at the uneaten food in front of me with pride, however, a sense of embarrassment washed over me as I glanced around the room and saw that the majority of the patients had finished their meal. 10% was my first meal completion, this number stung me and stayed in my brain for the rest of my time in treatment. After lunch I reunited with my mom and met with my care team which consisted of a new therapist, dietitian, and psychiatrist. We talked over my meal plan, treatment goals, the different stages of recovery, and what treatment would consist of.
The five stages of recovery: pre-contemplation, contemplation, preparation, action, and maintenance. For the first three weeks of treatment, I was in the pre-contemplation stage. Individuals who are in this stage are not ready for treatment, their mind is simply not thinking about it. They think that recovery is impossible and tend to justify their behavior by believing they are “not sick.” Day after day during intentions group – which was a group where patients would get to talk about their symptoms, challenges, and weekly goals – I vocalized my disinterest in recovery and treatment. Pre-contemplation, pre-contemplation, pre-contemplation. That was the only word I knew. I didn’t give myself the opportunity to open up and accept the help I was receiving. Instead, I tried so hard to tune everything out so I could keep the pain and comfort my eating disorder was providing me with. There was one moment early on in treatment where my psychiatrist had told me that it was time for me to start thinking about my discharge plan because my weight was “maintainable” and therefore I was “okay.” Yes, I was at a clinically stable weight but mentally I was nowhere near “okay.” Hearing from a doctor that my body weight was the determining factor as to whether or not I was stable enough to leave the program gave me confirmation that I didn’t have a problem because I wasn’t thin enough. I thought to myself, “why did I even come here if I’m okay?” “Why did I waste three weeks of my life here?” That same day I told my sister that I didn’t want to go back, I told her that I didn’t see how I could improve, I expressed the forbidden anger I felt by what the doctor had said. I was on the cusp of making the decision to skip treatment the next day, however, the real me knew I had to keep trying. I knew that I was here for a reason. I have an eating disorder no matter my body size. Eating disorders are not weight disorders, they are serious mental illnesses that can impact any person of any size, race, ethnicity, gender, sexuality etc.
“You can’t change the world on an empty stomach.” These were the words I heard while sitting across from my new individual therapist during our weekly sessions on Fridays. At first, I was scared to open up, I was scared to give talk therapy another try. I thought it would end up the same way as the first time – being let go. I didn’t want to be the challenging client who never takes the advice or never takes steps to change for the better, but in reality that’s exactly who I was for the majority of my time in treatment. I listened to everything my therapist had to say but I didn’t implement it into my life outside of the program. I chose not to. However, my therapist never gave up on me. As time went on, I developed a strong bond with my therapist. She was someone who I felt comfortable talking to about my life outside of treatment. I told her about my friends, school life, home life, future plans, passions, and she was the first person I told about my suicidal thoughts. She counteracted my negative thoughts and got me to sit in the uncomfortable feeling I was longing to avoid. With the help of my therapist and dietitian, I began to increase my meal completion slowly. I started to integrate more fear foods into my meal plan, I became more open with my group members, I started to communicate more with people in my life, I started to open my mind to the possibility of recovery. I tried so hard to shift my mindset because I knew that this was my only chance, I knew that if I denied the help I would never recover. I would never change my habits and that could put my future at risk. My therapist helped me see the impact my eating disorder had on my family, she helped me understand that the life I was living wasn’t actually life. She helped me realize that if I wanted to go to college, become a journalist, travel, and create change in the world, I would first have to create change within myself. This is when I slowly started to change the way I thought about treatment. In my sixth week of treatment I finally entered the third stage of recovery, the preparation stage.
Recovery isn’t linear. There will be days where you feel as if recovery is impossible but what’s important is how you react to that. The moment I thought I was doing good in recovery something always had to get in the way of my progress. Around my second to last week in treatment, I was moved down to IOP (intensive outpatient). This meant that I would only have to go to the hospital for three days out of the week and I wouldn’t have to attend the group zoom breakfast anymore. This was a big step for me. The time had come where I had to prove to myself and to my family that I was capable of implementing all the skills and habits I learned in treatment outside of program and into my real life. Before starting IOP you have to transition into something called taper days, this means that you get one day off from the program while transitioning from partial-hospitalization to intensive outpatient. My taper day sparked a new realization and commitment to recovery.
Friday – August 12, 2022
Before coming to program I really wanted to do college visits, especially Northwestern in Chicago. I was planning on doing the trip towards the end of August because I thought I would be out of program by then but I guess not. On Tuesday, I officially made up my mind about the visit and I started researching dates, flights, and hotels. I made a plan and wrote it down so I could share it with my family. I was really excited but when I told my mom about it I could tell she didn’t agree. Cost and weather were the reasons she came up with in order to steer me away from wanting to go.
“It’s so expensive over there. You can’t afford it.”
“How are you going to pay for it?”
“Scholarships are going to cut it.”
“The weather is worse over there than here in Oregon.”
I was not expecting this type of reaction from her. I was simply trying to tell her the plan and I wanted to see if she was on board, and clearly she wasn’t. It was upsetting hearing that from her. I realized it was my time to fight the internal battle of choosing between my family or my future. After that conversation, all my excitement about IOP and Northwestern faded away.
On Thursday during breakfast, my mom apologized for what she said and recognized that it wasn’t the best timing to bring those topics up. After all the progress I made I’m back to square one, I only ate about 25% of breakfast. [For lunch] I ate less than 50% and got two boosts. Same thing for dinner and I had nothing for my evening snack. I had my session with [my therapist] in the morning and it was really helpful. I am so grateful for her and all she has done for me. She doesn’t know how much her help and her words mean to me. I truly feel a sense of trust and support with her. We talked about this past week and how I wasn’t eating very much. We did an empty chair exercise where I pretended to talk to my mom while she wrote those things down for me to look back on. I told her how eating wasn’t important to me this week and that all I wanted to do was be alone. She told me that this path that I am building for myself isn’t working out for me and that it would eventually lead me to death. No more isolation, restriction, or bottling up emotions. It’s time to start taking action but it’s so hard. Same thing with [my psychiatrist], we had a really good conversation today. How I need to start letting go of my eating disorder. How I need to start doing the things that will benefit me and allow me to have the future I want to have. How I need to start getting angry at the voice in my head and start fighting back. My care team’s wisdom and insight really helped today, now it’s all up to me and honestly right now I have no motivation but I have to push through. For my family, for myself.
– M
My last two weeks of treatment were the hardest. This was the time when I finally accepted my treatment plan and entered the action stage, but it was also the time I realized that I had to let go of shadow. I realized that I had to move on. I had to nourish myself and put myself first because depriving myself of my needs wouldn’t work out in the long run. It was time to change my thinking and habits. I started eating 100% of my meal plan, contributing more to group discussion, and communicating with my family. I started to try more fear foods and even hung out with friends. I finally allowed myself to be seen by my family members and I attended all the family functions during those two weeks of treatment. By the last week of treatment, I knew that I wanted recovery for myself. I wanted to be able to eat cake, ice cream, chocolate, bread, salad dressing, rice, tortillas, tamales without the fear of what it would do to my body. I wanted to be able to be independent and go to college. I wanted to get my social life back and hang out with friends and family again without the fear of being judged. I wanted to start wearing clothes that made me feel good about myself. I wanted my hair to be shiny again and my skin to be soft. I wanted to stop feeling cold all the time. I wanted to get my life back, even if that meant gaining a couple of pounds. Body weight and physical appearance does not define you. I finally came to realize that on my last day of treatment.
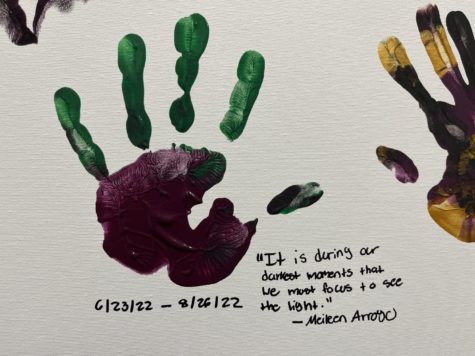
I was discharged from the program on August 26th, 2022. On a patient’s last day of treatment, they meet with their care team for the last time to discuss their progress in the program. Patient’s finalize their relapse prevention plan, add their hand print to the program canvas, and say their goodbyes. I remember being really emotional on my last day because I never thought that I would be able to make it nine weeks in the program. I was conflicted because I felt as if I wasn’t ready to leave just yet, but I also wanted to leave in time before my senior year started. I wanted a new door to open but I wasn’t ready to say goodbye to all the connections I had made in treatment. I had my last session with my therapist in the morning before the program started. During this time, we talked about my worries for the future regarding recovery, my progression in treatment, and what I learned from being in the program. When a patient discharges from the program they have a chance to share their recovery journey and experience in treatment to all the patients and staff through a synopsis. The synopsis can be a speech, song, art piece, or any other mode of expression. This was my synopsis:
June 24th was the beginning of the scariest yet most rewarding journey of my life. I had been silently struggling with an eating disorder and was never hospitalized or clinically underweight. How the media portrays eating disorders didn’t represent my experience at all and I fell into the massive lie that all eating disorders have a “look.” I told myself that because I was in a bigger body that meant that I didn’t have an eating disorder and that my family was wrong and I was right. I looked for validity in my statement: “I’m not sick and I don’t need help.” The confirmation to that statement was my body.
Coming into treatment, I didn’t feel deserving of my spot in the program. The majority of me was denying the help and didn’t want to spend my summer sitting in a seat for 4 hours of the day listening to important things I wanted to avoid and pretend didn’t exist. But there was a very faint part of me that wanted the help, that wanted to get better, and to let go of the self-hatred and harm that had become my identity and life. I spent the majority of my time here in pre-contemplation because I was too scared to get out of my comfort zone. I wanted to stay in my own little bubble away from the uncertainty that is real-life. I thought that recovering would lead me back to the body I used to have before my eating disorder. The body that was constantly put down and seen as “ugly and less deserving” by society’s beauty standards and my own internalized oppression.
As the days went by, I started to look at treatment in a more positive way. Thanks to my supportive purple group and my amazing therapist, I’ve learned that in order for me to recover I need to be okay with taking up space. I’ve learned that I deserve to enjoy my life, I deserve to be happy. I will admit that I’m still scared to fully let go of my eating disorder. I’m scared but I’m determined. That small little part of me that wanted to get better in the beginning of treatment is expanding. My time here in program is over but my future is still waiting to be written, by me and only me. I get to choose now, and I chose life. Even though it’s going to be the most uncomfortable, challenging, painful, and terrifying experience of my life…I’m willing to endure those uncomfortable feelings in order to feel comfortable in my own skin again.
To all the patients, I know comparison can be hard but your journey is uniquely yours. It might take a while for you to take action and do the hard things and that’s okay, it takes time. Don’t be afraid to express your emotions and talk about your experiences honestly, I promise everyone here understands and cares about you. This is more than a program, it’s a community and I will never forget this experience. Thank you!
– Meileen Arroyo
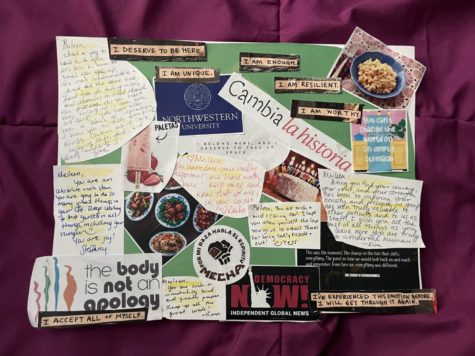
Treatment not only helped me start my recovery journey but it also allowed me to see that I wasn’t the only one who was going through a situation like this. Treatment helped me accept that I had a problem and through that experience I learned that it’s okay to seek help and guidance. I am extremely grateful that my mom made the decision to enroll me in the program because if she hadn’t I really don’t know where I would be right now. I probably wouldn’t have written this story or been alive to share it. I have so much appreciation for my family and their support. Currently, I continue to see an individual therapist, dietitian, and my primary care provider for weights and vitals check-ins. I have been in the recovery process for 10 months now and although I am so proud of the improvement I have made. I still have days where I have no motivation. I still deal with intense body image issues, food anxiety/guilt, and comparison, but because of treatment I have the skills to be able to bounce back from low days and negative thoughts.There are times where my eating disorder voice is too loud to handle and I slip back into my unhealthy coping skills but I never let those “bad” days define my progress in recovery. Sometimes it seems like there’s nowhere else to go with recovery and sometimes I fall back into the “I’m fine” mentality but I know that isn’t me who’s talking. It’s the deadly eating disorder voice that wants me to hold on, but in order to live my life freely I can’t keep listening to the voice. I can’t let my eating disorder control me anymore, it’s time for me to take control of it instead. After three hard years of struggling in silence, I finally am ready to speak out and share my story. I wanted to show people that behind a smiling face there can be so much pain and destruction. I wore a mask for the longest time but I am now finally able to take it off and talk about my experience freely without shame. If you are someone who is struggling with an eating disorder I hope you know that you are not alone. You have people who care about you and who want to help you get better. Recovery is tough and terrifying but it is also rewarding and special. It is never too late to ask for help, it is never too late to get your life back, it is never too late to be yourself again. Because of recovery, I am now able to say: My name is Meileen Arroyo and I have been struggling with an eating disorder for three years now.
ANAD Free Eating Disorder Peer Support Groups